The recent discovery of a process in fruit flies connecting inflammation with impaired motor function sheds light on a potential target for alleviating the persistent muscle fatigue experienced by individuals with long COVID. This finding is especially significant given that one of the most debilitating symptoms of long COVID is an intolerance to exertion. According to Washington University developmental biologist Aaron Johnson, the reduction in energy levels in skeletal muscle due to inflammatory processes can significantly decrease the capacity to move and function normally.
With each new infection of the SARS-CoV-2 virus, the risk of developing long COVID increases, leading to a variety of physical symptoms, including muscle fatigue. Approximately 18 million American adults have encountered the lingering malaise associated with long COVID, with many experiencing a loss of energy that affects nearly half of all long COVID sufferers. It is important to note that muscle fatigue is not only common in long COVID patients but also in individuals with other post-viral conditions and neurodegenerative diseases like Alzheimer’s and Parkinson’s, all of which involve inflammation of the central nervous system.
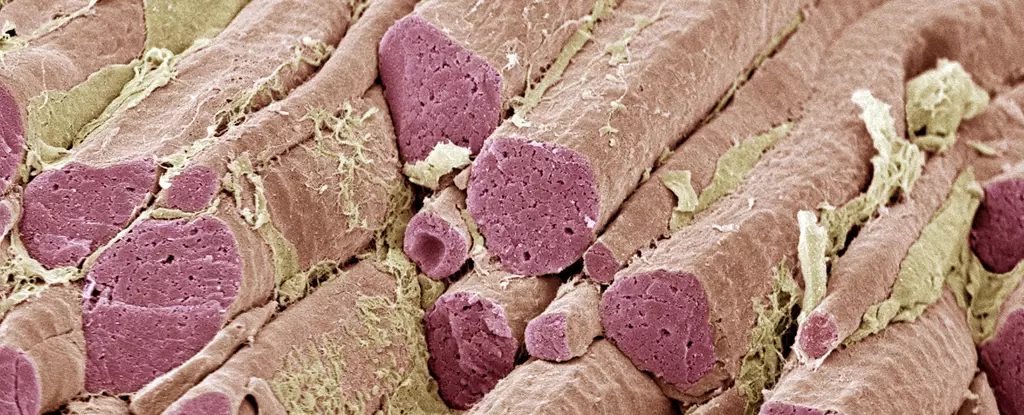
Researchers at Washington University utilized animal models to investigate how inflamed neurons can lead to impaired muscle function. By identifying a signaling pathway between brain cells and muscles in both flies and mice, the researchers uncovered a mechanism that results in reduced motor function. The presence of COVID-associated proteins in the brain led to decreased muscle performance in the test animals, indicating a direct correlation between brain inflammation and muscle dysfunction across various disease categories.
In humans, inflammation triggers the release of the immune cytokine interleukin-6 (IL-6) by neurons, which then travels to muscles via the bloodstream and activates the JAK-STAT cellular program. This activation suppresses energy production in muscle tissues, affecting their ability to function properly. Despite uncertainty about why the brain produces a protein signal that impairs muscle function, researchers speculate that it may serve as a mechanism to reallocate resources during times of illness. Further research is needed to fully comprehend this process and its implications for the body.
By blocking the JAK-STAT pathway in flies through the use of drugs, researchers were able to reverse the muscle dysfunction observed in their experiments, offering hope for potential treatment strategies. IL-6 inhibitors, already used to treat autoimmune diseases like rheumatoid arthritis, have shown promise in managing severe cases of COVID-19. The persistence of cytokine signaling in the brain-muscle axis even after the resolution of the initial infection suggests that long COVID may be a result of chronic inflammation.
Despite the remaining uncertainties surrounding how SARS-CoV-2 enters the central nervous system to induce inflammation, this new insight into the link between inflammation and impaired motor function presents an opportunity for alleviating the symptoms of various chronic conditions. By targeting the chemicals released by neurons, researchers can now better understand how brain inflammation impacts the entire body, paving the way for improved treatment approaches.

Leave a Reply