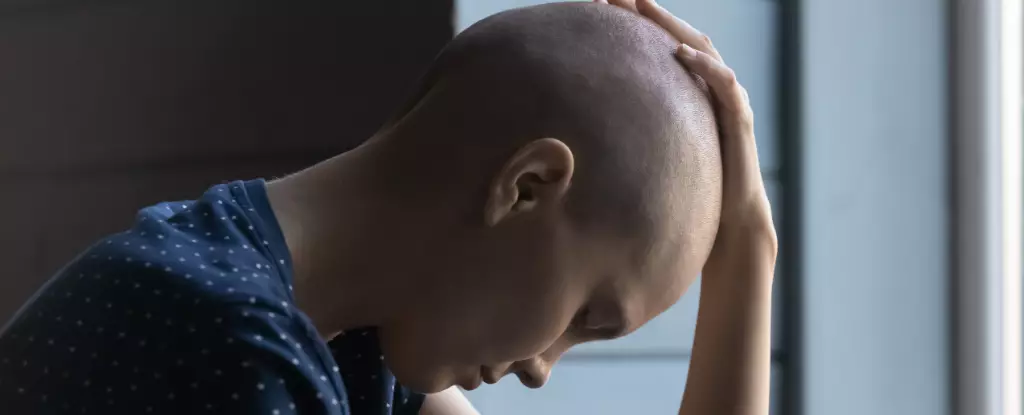
Advanced cancer relentlessly ravages not only the body but also the mind. While the physical ramifications, such as weight loss and muscle wasting, are often addressed, the insidious side effect of apathy remains obscured in the shadows. Patients diagnosed with late-stage cancers frequently find themselves engulfed by a profound disinterest in activities that once enriched their lives—an emotional toll that exacerbates the suffering caused by their physical illness. This psychological phenomenon isn’t merely a reaction to despair; it’s a manifestation of a biological process that may stem directly from the cancer itself.
Commonly referred to as cachexia, this syndrome affects a staggering 80% of patients in advanced stages of cancer. It results in significant weight loss and muscle degeneration despite adequate nutrient intake. Sadly, this pervasive apathy leads to isolation—not just from activities and interests but also from families and communities—making a tough journey even more daunting. In clinical settings, physicians often attribute a patient’s withdrawal to psychological distress caused by illness. But what if apathy is more than an emotional response? Recent groundbreaking research suggests it may be a direct consequence of cancer’s interaction with the brain’s motivational circuits.
Unraveling the Mysteries of Apathy in Cancer
In a confluence of neuroscience and oncology, an intriguing study reveals that cancer doesn’t simply deplete bodily resources; it actively disrupts brain functions responsible for motivation. The researchers employed advanced methodologies typically reserved for animal studies—utilizing mouse models to probe the depths of this complex interplay. As cancer progresses, the tumors release inflammatory molecules, known as cytokines, into the bloodstream, effectively hijacking neural pathways that regulate our drive to engage with the world.
Critical among these pathways is a brain region called the area postrema. Unlike other brain areas shielded by the blood-brain barrier, this region can directly interact with inflammatory signals flowing through the bloodstream. When it senses an uptick in these signals, a cascade effect occurs, reducing dopamine levels in key motivational centers of the brain, ultimately daunting the human spirit and diminishing the will to act.
The neurobiological ramifications of this discovery are profound: dopamine, often misrepresented as merely a “feel-good” hormone, is fundamentally aligned with our ability to strive, to engage, and to reap rewards. Dishearteningly, as cancer progresses, the suppression of this critical neurotransmitter leads to a stark decline in patients’ motivation, mirroring the sentiments expressed by patients who find even simple tasks dauntingly exhausting.
Reversing the Dark Tide of Apathy
However, the study does not just shed light on the disheartening mechanics of cancer-induced apathy; it also uncovers potential avenues for reversing this debilitating condition. By manipulating the function of the inflammation-sensing neurons in the area postrema, researchers were able to revive motivation in mice, creating a glimmer of hope for patients battling similar symptoms in humans.
Additionally, the research introduced the possibility of pharmacological interventions targeting specific inflammatory responses—akin to existing treatments for rheumatoid arthritis—to reestablish a sense of drive. Although the physical deterioration continued unabated, these findings herald a new approach to enhancing the quality of life for patients enduring the harrowing realities of cancer treatment.
Apathy, often regarded as an inevitable companion of chronic illness, now presents itself as a tangible target for intervention. The potential to intercept inflammatory signals and re-engage motivational circuits offers an exciting prospect not only for cancer patients but for individuals grappling with a range of chronic diseases driven by similar inflammatory mechanisms.
The Broader Implications of Inflammation-Induced Apathy
The implications of this research extend beyond the realm of oncology. The inflammatory mechanisms uncovered are also involved in various other debilitating conditions, including autoimmune diseases and chronic infections, indicating that apathy is not exclusive to cancer patients. Millions of individuals suffering from chronic illnesses might silently endure this loss of drive, further complicating their recovery and overall well-being.
Interestingly, this biologically-rooted apathy might have evolved as a survival mechanism, conserving energy during acute illness. But when inflammation becomes a chronic state, as seen in cancer, this once-protective feature transforms into a barrier to wellness, leading to prolonged suffering and diminished quality of life.
Arming ourselves with a deeper understanding of the intersection between motivation and disease opens the door to innovative treatment opportunities. By isolating and targeting the inflammatory pathways disrupting motivation, researchers can pave the way for therapies that may one day help reclaim the vitality and engagement that chronic illness seeks to extinguish.
The path ahead is laden with challenges, but for patients and families witnessing the slow erosion of their loved ones’ will to live fully, these scientific breakthroughs illuminate a potential route to recovery—a chance to rediscover the spark of life even in the throes of illness.

Leave a Reply