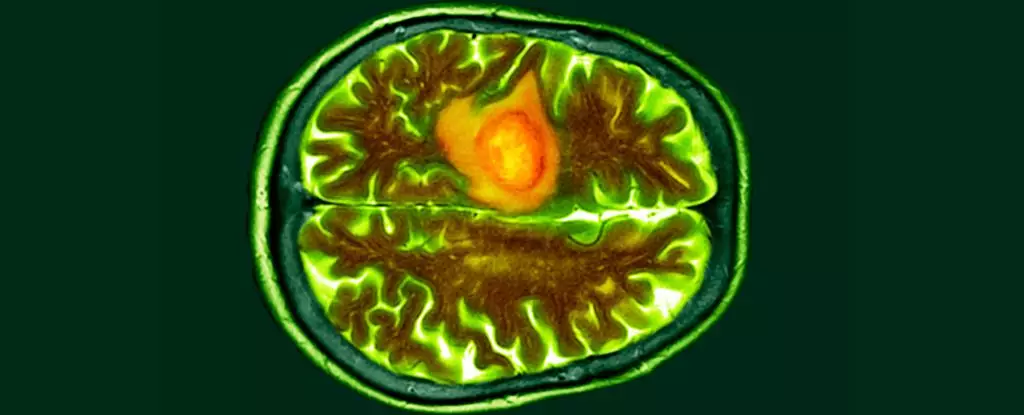
In a groundbreaking development, scientists have unveiled a new method for detecting brain cancer that is not only incredibly fast but also significantly less invasive than traditional surgical biopsies. This innovative ‘liquid biopsy’ technique requires only 100 microliters of blood and can identify biomarkers associated with glioblastoma – the deadliest form of brain tumor – within just one hour. The accuracy and efficiency of this new approach far surpasses all existing tests and markers for glioblastoma, making it a remarkable breakthrough in the field of cancer diagnosis.
This cutting-edge liquid biopsy was developed by a collaborative team of researchers from the University of Notre Dame in the United States and Australia. The test is based on the detection of mutated blood biomarkers known as epidermal growth factor receptors (EGFRs), which are commonly overexpressed in various cancers, including glioblastoma. These biomarkers are encapsulated within extracellular vesicles – small packages that contain proteins, lipids, and genetic material from their parent cells. By leveraging the specific characteristics of these extracellular vesicles, the researchers were able to design a sensor that can identify the presence of mutated EGFRs in the blood with exceptional sensitivity.
The core technology driving this liquid biopsy is a biochip equipped with a supersensitive sensor coated with antibodies that target exosomes carrying mutated EGFRs. This biochip, which costs less than $2 to produce, allows for direct testing of untreated blood plasma samples without the need for prior isolation of extracellular vesicles. When mutated EGFRs bind to the chip’s antibodies, a voltage change occurs in the plasma, generating a distinctive negative charge that indicates the potential presence of cancer. In clinical trials involving blood samples from glioblastoma patients and healthy individuals, the biochip demonstrated outstanding accuracy in detecting cancer biomarkers, highlighting its potential as a reliable diagnostic tool.
Potential Implications and Limitations
The ability of the biochip to quantify exosome concentrations even at low levels opens up new possibilities for cancer research, biomarker discovery, and disease monitoring. However, the researchers acknowledge that there are some challenges to be addressed. Mutated EGFRs are not exclusive to glioblastoma and are also associated with other types of cancers, such as colorectal cancer. This poses a limitation in using EGFRs as specific indicators of glioblastoma, as patients with the disease may exhibit different forms of EGFR alterations.
To refine the specificity of the liquid biopsy test and differentiate between various types and stages of cancer, the researchers propose conducting extensive studies on larger cohorts of glioblastoma patients. By analyzing the unique biomarker profiles present in the blood of these patients, the team aims to develop a more tailored diagnostic platform that can accurately identify different types of cancer and determine their progression stages. Scaling up the current testing platform to accommodate a broader range of cancer patients will be crucial in establishing comprehensive profiles for various cancers.
While the new liquid biopsy method represents a significant advancement in the early detection of brain cancer, further research is needed to enhance its diagnostic capabilities and address the challenges associated with identifying specific cancer types. The potential of this technology to revolutionize cancer diagnosis and monitoring is promising, and with continued innovation and refinement, it has the potential to transform the landscape of cancer detection and treatment.

Leave a Reply