In medical emergencies, particularly cardiac arrests, the minutes following an incident can be pivotal. Cardiopulmonary resuscitation (CPR) significantly enhances the likelihood of survival, by maintaining blood circulation and supplying oxygen to vital organs until emergency services can take over. Despite this, statistics reveal a disturbing trend: bystanders are less inclined to perform CPR on women compared to men. This gender disparity raises crucial questions about societal attitudes and preparedness surrounding life-saving interventions.
A study conducted in Australia examined nearly 4,500 cases of cardiac arrest from 2017 to 2019 and highlighted that only 65% of women experiencing cardiac arrests outside of hospitals received CPR compared to 74% of men. This gap suggests a systemic reluctance to assist women in critical situations, which can have dire consequences for their chances of survival.
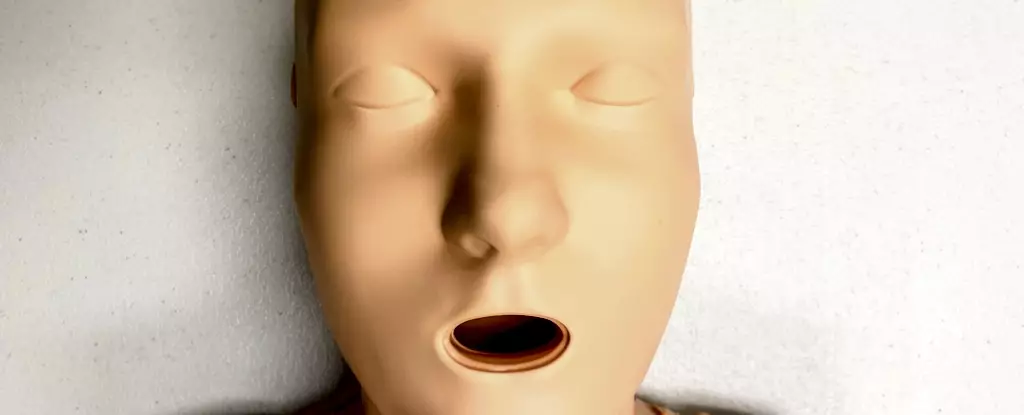
One significant factor that may contribute to this difference in response rates is the design of CPR training dummies, traditionally referred to as manikins. A comprehensive analysis of CPR training resources revealed that a staggering 95% of these manikins do not represent the anatomical diversity that exists in reality. Most are designed with flat chests, which not only fails to reflect the actual bodies of many potential patients but may also implicitly convey a default notion of masculinity.
While the technique to perform CPR remains unchanged across genders—breasts do not alter the manual method—this lack of diverse representation could deter bystanders from acting, especially in moments of high stress and uncertainty. The striking underrepresentation of female bodies in CPR training creates a subconscious bias that may influence individuals’ willingness to intervene.
The implications of these findings extend beyond just the failure to provide CPR. They are symptomatic of a broader issue of gender bias in healthcare, where women and marginalized genders, including transgender and non-binary people, frequently face disparities in treatment. Research indicates that women are more likely to have their symptoms dismissed or misdiagnosed, often leading to delayed diagnoses and interventions. This systemic bias is harmful, as it perpetuates unequal health outcomes in critical situations like cardiac emergencies.
Compounding the problem is the societal stigma surrounding potential accusations of sexual harassment. Bystanders may hesitate to approach women in distress due to fears of misinterpretation of their intentions or discomfort with certain physical interactions. This hesitation is particularly detrimental in life-or-death situations where time is of the essence.
To improve the response rates of bystanders, it is crucial to diversify CPR training materials. Addressing the anatomical diversity of CPR manikins is a step that must be taken seriously by training organizations. Research conducted in 2023 identified 20 CPR manikins available globally, of which only five were marketed as “female,” and only one of those had breasts. This stark reality emphasizes a dire need for manufacturers to design training manikins that accurately reflect the demographics they educate about.
Furthermore, while many CPR training courses do not specify the sex of the manikins used, their flat-chested design ultimately reinforces a male-centric view of medical emergencies. This lack of meaningful representation can signal to learners that only men require urgent medical assistance, thus perpetuating misconceptions that ultimately hinder women’s health outcomes.
Education plays a critical role in changing the narrative surrounding CPR and its execution. Communities must be trained not only to recognize the signs of cardiac arrest, such as a person not breathing or failing to respond, but also to feel empowered to act without fear of social stigma. Effective CPR training should emphasize the crucial point that the act of saving a life outweighs potential discomfort.
Additionally, it is vital for training programs to illustrate that CPR can and should be performed on individuals of varying body types. Participants must learn that time is of the essence, and unnecessary hesitation—or social anxieties—can result in tragic outcomes.
The need for better representation in CPR training materials and a deeper understanding of gender biases in health responses is urgent. By making deliberate changes to training resources and enhancing public education around CPR, we can increase bystander intervention rates, ultimately saving lives. It is imperative to foster a culture that prioritizes effective medical assistance over societal hesitations, ensuring that everyone—regardless of gender—receives the care they need and deserve.

Leave a Reply