Recent research conducted by a team of scientists in China has unveiled a remarkable breakthrough in our understanding of brain recovery following cardiac arrest. The study highlights an innovative approach to reviving brain function in pigs, demonstrating that significant neuronal activity can be restored up to nearly an hour after circulatory cessation. This groundbreaking work not only holds promise for a deeper understanding of the intricacies of post-cardiac arrest recovery but also suggests that medical professionals may have more time to administer resuscitation methods to patients experiencing sudden cardiac events.
Central to this research is the hypothesis that integrating an undamaged liver into the life support system could enhance the likelihood of restoring brain function after ischemic events. Cardiac arrest leads to a rapid shutdown of blood flow, resulting in global ischemia, which can cause devastating effects on the brain within minutes. The discovery that the liver can play a supporting role in mitigating these effects opens up new avenues for therapeutic interventions.
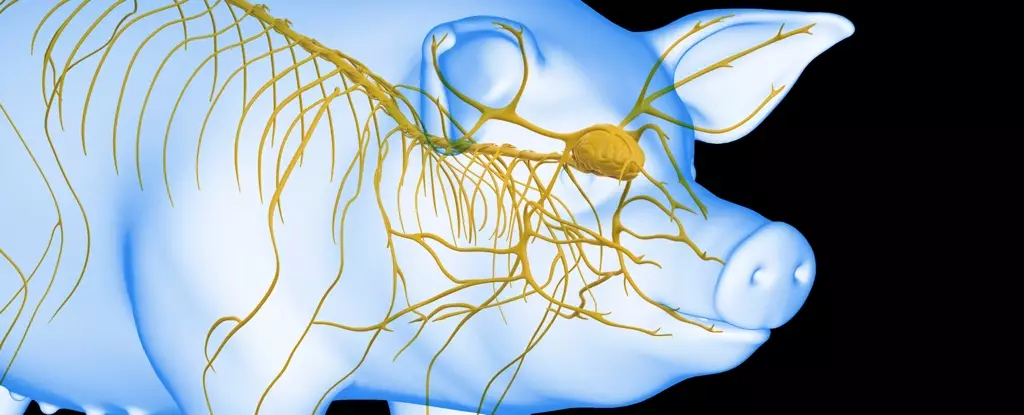
The liver, often overlooked in discussions about multi-organ failure, experiences its significance in the context of brain ischemia. Prior theories suggested that brain recovery hinges solely on the brain’s condition without investigating the contributions of other organs. In this study, the researchers employed 17 Tibetan minipigs to systematically investigate the effects of liver ischemia on brain health after induced circulatory arrest.
The experimental design was meticulous: the pigs were subject to a 30-minute period of brain ischemia, with one group also experiencing liver ischemia. A control group that underwent no ischemia was also included for comparative analysis. Post-experimentation, the evaluation of brain tissues revealed a striking contrast in damage levels between the groups. The group without liver ischemia exhibited significantly reduced brain damage, underscoring the protective potential of the liver during ischemic events.
Following the initial findings, the researchers ramped up their approach by implementing a life support system that integrated an undamaged liver. This system involved an artificial heart and lung apparatus designed to pump fluid through the brain, simulating conditions that could be used in medical settings.
Significantly, the experiments commenced at intervals after cessation of blood flow, revealing crucial insights into how timing and liver functionality influence the likelihood of reviving brain activity. Notably, when brain tissues were connected to the liver-assisted life support system just ten minutes after resuscitation commenced, a resurgence of electrical activity was evident. However, the most promising outcomes emerged when connections were made 50 minutes after blood flow had ceased, resulting in sustained brain activity for up to six hours.
These findings emphasize a critical time window for resuscitation success and highlight the complex interplay between the liver and brain during recovery efforts. Strikingly, even in models where the brain had been deprived of oxygen for a full hour, some degree of activity could be reinstated, albeit for a shorter duration.
The implications of these findings extend well beyond animal models. As cardiac arrest remains a leading cause of mortality globally, advancements in resuscitation practices are paramount. The elucidation that the liver can act as an auxiliary support system paves the way for next-generation resuscitation techniques that consider organ interdependence rather than isolating treatment to the brain.
Future research will undoubtedly focus on translating these insights into human applications, examining whether similar protocols can improve outcomes in real medical scenarios. Expanding our understanding of the liver’s role in neurological recovery may lead to innovative strategies that extend the viable window for effective resuscitation.
The exciting path of this research reveals a profound opportunity to enhance medical protocols concerning cardiac arrest, ultimately aiming to improve survival rates and quality of life for patients. As we venture deeper into the mechanisms of multi-organ involvement post-arrest, the potential for transforming cardiovascular medicine becomes increasingly tangible. The findings serve as a catalyst for further exploration into organ systems and their collaborative efforts in maintaining human health during critical medical emergencies.

Leave a Reply