Cognitive function in patients suffering from mood disorders has garnered significant attention recently, particularly in relation to the long-term effects of medications like selective serotonin reuptake inhibitors (SSRIs). These drugs are widely prescribed for treating anxiety and depression, yet their therapeutic efficacy remains a matter of contention within the psychiatric community. A notable study spearheaded by psychologist Vibeke Dam from Copenhagen University sheds light on the intricate relationship between SSRI use, cognitive improvements, and serotonin receptor activity, especially concerning the 5HT4 receptor.
In a meticulously designed study involving 90 participants diagnosed with moderate to severe depression, researchers utilized brain scans and cognitive assessments to gauge the effects of the SSRI escitalopram over an eight-week treatment period. This dual approach aimed to elucidate not just the clinical symptom alleviation but also the cognitive advancements attributable to the medication.
Initial assessments established baseline metrics, subsequent to which participants were administered daily doses of escitalopram. Follow-up evaluations included repeated brain scans and cognitive tests conducted at the conclusion of the treatment period, culminating in assessments at week 12. The results presented a noteworthy finding: a reduction of nearly 10 percent in the binding of serotonin receptors post-treatment, coupled with significant gains in verbal memory performance among patients. Particularly, those with the least change in 5HT4 receptor activity exhibited the most pronounced cognitive benefits.
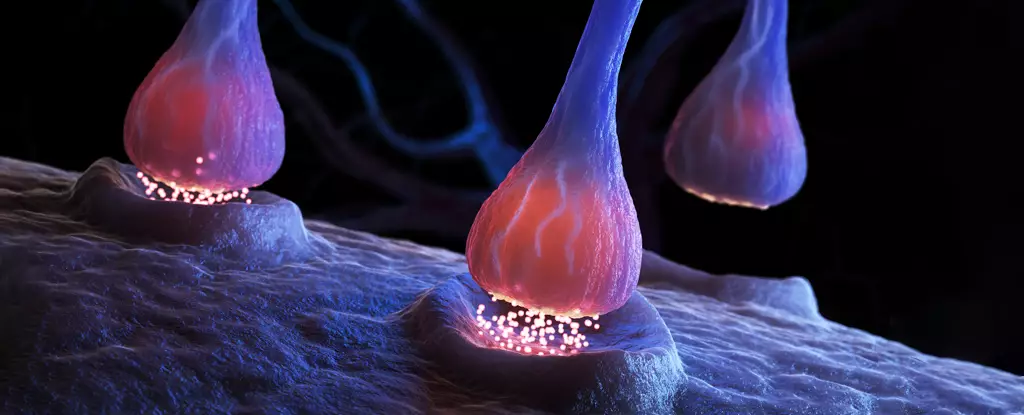
Perhaps the most striking revelation from Dam’s study is the dissociation between mood enhancement and cognitive improvement. While the subjects experienced a degree of alleviation in depressive symptoms, alterations in the serotonin receptor profile did not align with these mood changes. This disjoint raises fundamental questions about the mechanisms through which SSRIs operate, particularly as existing evidence suggests that these medications might enhance serotonin levels in synapses, thereby optimizing the efficiency of remaining receptors.
Dam’s recognition of the 5HT4 receptor as a pivotal target for cognitive function enhancement highlights a critical area for future research. Notably, prior research indicated that both unmedicated individuals with major depressive disorder and healthy individuals with familial depression risk possessed fewer of these receptors, suggesting a correlation between receptor quantity and memory issues common in depression. Nevertheless, the implications of this study beg for further investigation to validate these findings and their practical applications.
Yet, despite these promising outcomes, the study’s design was not without its ethical implications. Limitations in utilizing a placebo-controlled structure cast a shadow on the conclusiveness of the results. Without a control group, one cannot definitively attribute cognitive improvements solely to the SSRI use, as confounding variables may arise. Furthermore, skepticism surrounding the efficacy of SSRIs as a treatment modality for depression persists, spurred by studies suggesting that these medications may not outperform placebos. This raises critical considerations regarding the very foundation of serotonin’s role in mood disorders.
Despite the findings, it is imperative not to draw hasty conclusions about SSRIs’ utility in treating depression or cognitive impairment. The discussion necessitates a balanced approach, particularly regarding patient safety, as discontinuing SSRIs without medical consultation can provoke serious withdrawal symptoms. Given the significant reliance on these medications for managing mood disorders, ongoing research aimed at unraveling the complexities of their action remains vital.
Froekjaer’s call for future studies to illuminate the mechanisms behind antidepressants highlights the pressing need for advancements in precision psychiatry for individuals navigating major depressive disorder. As research continues to evolve, so too must our understanding of the broader implications of these findings, particularly concerning personalized treatment strategies for mental health.
While the recent findings related to SSRIs and cognitive function offer a glimpse into the potential benefits of these medications beyond mood relief, they also underline the pressing need for more thorough investigations into their mechanisms. As psychiatric research delves deeper into understanding the relationship between serotonin receptors and cognitive capabilities, it opens avenues for optimizing therapeutic interventions. The journey towards debunking myths and enhancing treatment methodologies in mental health underscores the importance of an informed, nuanced conversation around SSRIs and their role in combating mood disorders.

Leave a Reply