The debate surrounding the impact of circumcision on reducing the risk of HIV infection among men who have sex with men has been ongoing. A recent randomized controlled trial conducted by researchers from Sun Yat-sen University in China aimed to provide further insight into this issue. The study compared two groups of men who voluntarily underwent circumcision over a twelve-month period, using blood tests to assess the impact on HIV transmission.
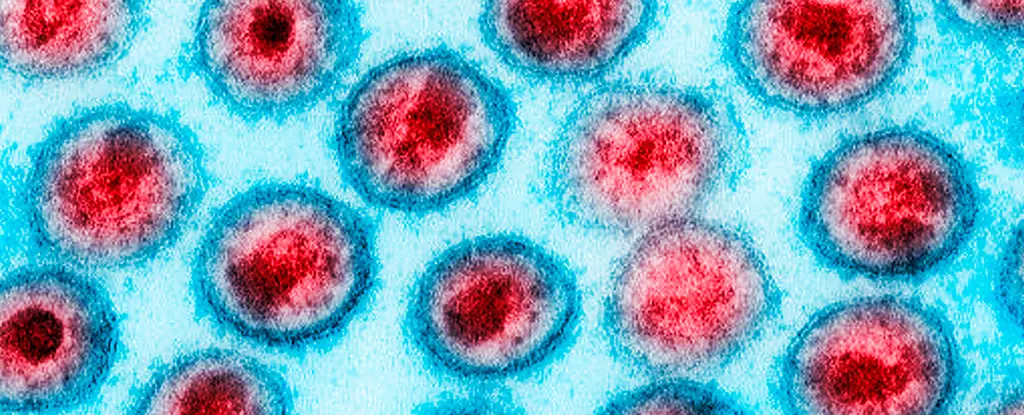
HIV remains a significant public health threat globally, particularly in some parts of the world where hundreds of thousands of lives are claimed each year. While the death rate has decreased since the early 2000s, certain regions, especially in Africa, continue to bear a disproportionate burden. Despite advancements in treatment and prevention efforts, there is still no cure for HIV. Research suggests that circumcision may play a role in reducing the risk of HIV transmission, in addition to other sexually transmitted infections.
The study involved 247 uncircumcised men between the ages of 18 and 49 from various cities in China, all of whom were HIV-seronegative. Participants reported engaging in primarily insertive anal intercourse and having multiple male sex partners. The men were randomly assigned to either the intervention group, where circumcision was immediately performed, or the control group, where circumcision was delayed for a year. The results showed no seroconversions in the intervention group, indicating no new HIV infections among these men. In contrast, the control group experienced five seroconversions during the study period.
While the findings of the study are significant, there are limitations to consider. The sample size was relatively small, and the overall rate of HIV infection was lower than anticipated. Additionally, the practice of circumcision, particularly when performed on minors without their consent, remains controversial. Campaigns promoting circumcision for HIV prevention in Africa have faced criticism for cultural insensitivity and lack of contextual research.
The research suggests that voluntary medical male circumcision could offer some level of protection against HIV infection for men who have sex with men. However, the authors of the study caution against overemphasizing the role of circumcision as a standalone preventive measure. Comprehensive protection against HIV should involve a combination of strategies, including safe sex practices, testing, and education.
While circumcision may have a role in reducing the risk of HIV transmission among men who have sex with men, it is crucial to approach this issue with sensitivity and consideration for cultural differences. More research is needed to fully understand the impact of circumcision on HIV prevention, and efforts should focus on comprehensive and inclusive strategies to address the complex challenges posed by the HIV epidemic.

Leave a Reply